As you know, anaesthesia has a lot of similarities to aviation, in that both are very safety oriented fields. Something that pilots and anaesthetists have in common is that both monitor lots of vital parameters. Below is the cockpit of a modern passenger aircraft about to land. You see various screens which show all sorts of parameters, that the pilots have to monitor.

In anaesthesia too, we have lots of vital parameters that we have to constantly monitor.
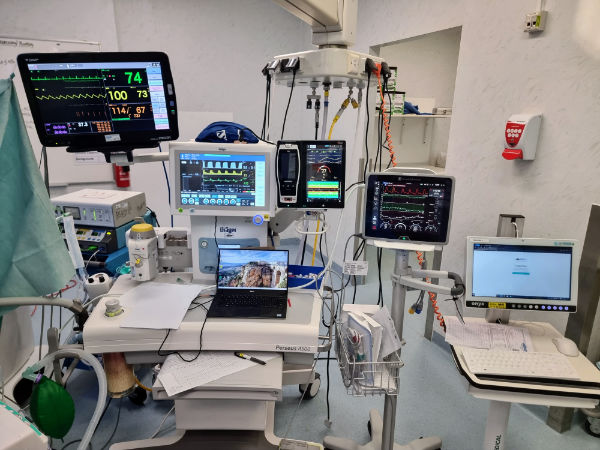
When there are many vital parameters to monitor, it is easy to forget monitoring some of them. If one looks at various parameters randomly, there is a chance that some will be missed.
In aviation, to avoid forgetting to monitor some parameters, pilots do not randomly look at the various parameters. Instead, they use a systematic way of looking at them and they call it “scanning”. With scanning, since the pilots look at the parameters in an orderly way, so that they do not miss anything.
As mentioned before, just like pilots, we anaesthetists need to constantly monitor many vital parameters. And like the pilots, if one develops a standardised way of looking at parameters of our anaesthetised patients, it can help one to not miss any of them. In the next sections, I will share with you the scanning system that I use. I call my scanning system, “Rapid Anesthesia Scan” (RAS), and it can help you to be more thorough when monitoring your anaesthetised patients.
I am sharing the Rapid Anesthesia Scan with you only to demonstrate the concept. It is not meant to be a definitive system. If you choose to use it, please do so at your own risk! Once you understand the concept, you can of course modify it to suit your preferences.
I do not do the rapid scan every single minute. Rather, like lots of anaesthetists, I often do randomly look at the monitors, glancing at the blood pressure, ECG, etc. But at intervals, I decide to do the full scan, so that I can reassure myself that I have looked at everything. I also do the rapid anaesthesia scan whenever I take over a case, for example when I give breaks to my colleagues.
Now let me share with you, the Rapid Anaesthesia Scan (RAS).
To make RAS easy to remember, I have modified the typical ABCDE approach we do when assessing trauma patients.
Airway:
I start the scan by looking at the airway and the breathing system tubes connected to it.
I check that the breathing is connected well at the machine end and the airway end.
I then check the airway itself, to see if it has got displaced or kinked, etc.
Breathing:
As you know, the two gases that are relevant for respiration are oxygen and carbon dioxide.
For oxygenation, I look at saturation and then look at the FiO2.

I then look at ETCO2 and look at ventilation. For ventilation, I look at Fresh Gas Flow, Airway Pressure, Volume, Rate, PEEP, etc.
I then think of the physical lung. Is it being equally ventilated (If intubated, I normally auscultate at start). At the bottom of the lung, I think of the diaphragm, which reminds me to check for enough muscle relaxation.
Circulation:
I often think of the cardiovascular system like this diagram. I.e. there is an output, the heart itself, and fluid status (preload).
I start with output. For most of my cases, it’s blood pressure that tells me the output.
Then I think of the heart itself, i.e. the heart rate and ECG/EKG

Then I move onto fluid status (preload). I think of what is going into the vascular system, i.e. fluids.
I then think of what is leaving the vascular system, e.g., blood loss, urine output.
If you have additional cardiovascular monitoring, (e.g. CVP, cardiac output monitor) you can incorporate them into your scan.
Depth:
In advanced trauma life support, the D stands for disability. For the anaesthesia scan, I modify this to mean “depth of anaesthesia”.
I will look at end tidal measurements of gases, and see if the vaporiser has enough agent.
I look at the TCI pump settings.
I will look at the depth of anaesthesia monitor.
Environment:
I check patient temperature, pressure points, and mechanical calf compression pumps.
As mentioned at the start, initially this scan may look complicated. But in reality, once you do it a few times, you will find it very easy and quick.
As you start using a scanning practice, you will discover things here and there that you have missed. I hope you find it as useful as I do. Please share this with other anaesthetists near and far. Thank you.
You can leave a comment for me to see by clicking here